Introduction
By: Matthew Zubiller, CEO, e4health & David Van Doren, Partner & Board Member e4health
Addressing inefficiency in healthcare’s administrative and operational processes is the optimal launch point for the use of artificial intelligence (AI), machine learning (ML), and robotic process automation (RPA) in hospitals and health systems. Specifically, addressing a messy mid-revenue cycle can be a quick win to achieve value through automation.
The use of AI, ML, and RPA in the mid- revenue cycle enables staff to work smarter, not harder. Intelligent bots serve as digital copilots alongside revenue cycle staff to achieve essential goals:
- Optimize net revenue and accelerate cash
- Prevent denials and ensure quality
- Enhance team member productivity
However, not all intelligent automation is equal, with few proven use cases implemented at scale. As healthcare executives are presented with a variety of AI solutions in 2024, they must understand the fiscal impact of those options to guide their decisions.
New technologies will provide real opportunities for net revenue enhancement, accelerated cash, and cost-savings, but likely also come with a significant investment of time and resources. Choosing the wrong technology partner can at best delay value realization, and at worst have a dramatic impact on cash, costs, DNFB and net realized revenue.
This executive brief separates myth from reality in mid-revenue cycle AI, ML, and RPA solutions while providing a trustworthy, step-wise approach to the selection and use of these next generation technology tools.
Did you know that 74% of healthcare organizations (HCOs) automate some portion of their revenue cycle operations, with 46% of these HCOs going beyond RPA to use AI or ML. Among organizations not using automation, 80% plan to do so by the end of 2025.
Click here to download a PDF copy of this executive summary.
Separating Myth from Reality: What’s Real and Effective Today
According to Harvey Castro, MD, MBA, author of ChatGPT and Healthcare, the use of ChatGPT, a commonly used generative AI system, reached the summit of Gartner’s “peak of inflated expectations” in the summer of 2023. However, position at the top of the cycle only means one thing. The technology is poised for a fall into Gartner’s “trough of disillusionment.”
In 2024 it is crucial for healthcare executives to acknowledge the potential pitfalls of nascent technology in healthcare. As Dr. J. Peterson notes, “You don’t know what biases and errors are being built into the systems. This is an unbelievably major source of current threat.”
While we are genuinely excited about the path ahead, health executives must remain grounded in reality. The value from AI in healthcare will take time, resources, and investment while progressing iteratively and leveraging industry expertise.
This is where e4health’s unique strength lies—matching sophisticated technology with the human component. Our experts keep a watchful eye, ensuring that new technology doesn’t inherit and perpetuate legacy system biases. By combining AI with human oversight, we strive for a balanced and ethical approach to automation in the mid-revenue cycle.
Three Red Flags to Know
1. The very nature of AI lies in its construction and training, raising concerns about inherent biases introduced during development.
2. Individuals creating these systems play a pivotal role, and their biases can inadvertently shape AI outputs.
3. Lack of involvement by human subject matter experts with mid- revenue cycle expertise hinders the effectiveness of new AI solutions and puts value realization at risk.
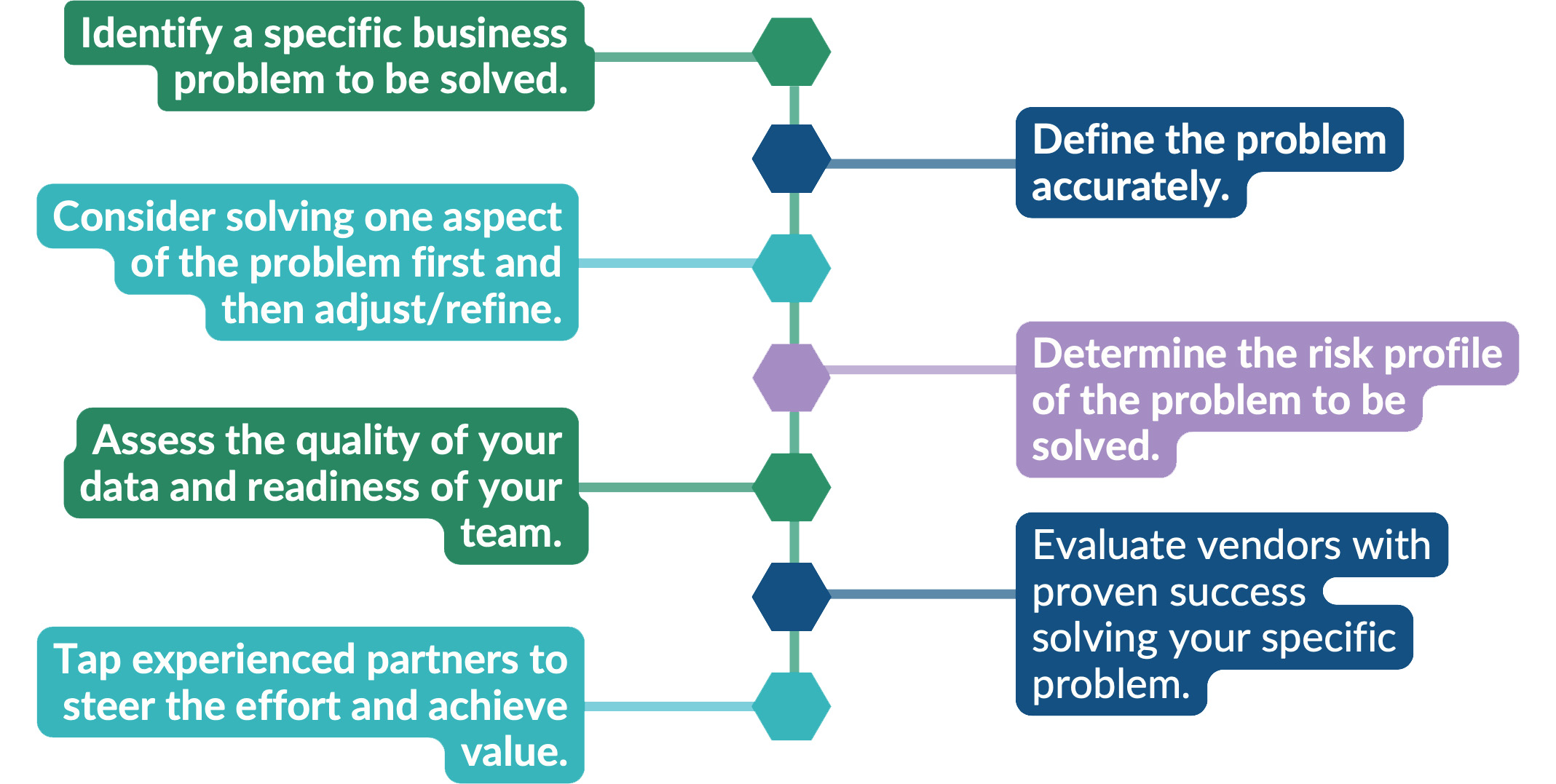
Take a Problem-Based Approach to Mid-Revenue Cycle Automation
e4health’s depth of experience and expertise with healthcare technology and within the revenue cycle provides a valuable guide for HCOs as they evaluate AI, ML, and RPA solutions to drive automation, improve net revenue realization, accelerate cash, and reduce cost.
AI outperforms humans in some mid-revenue cycle tasks, but not all. Therefore, a problem- based and step-wise approach to the implementation of these technologies is essential. The journey begins by asking the right questions and solving the right problems.
Proven Use Cases for Mid-Revenue Cycle Automation
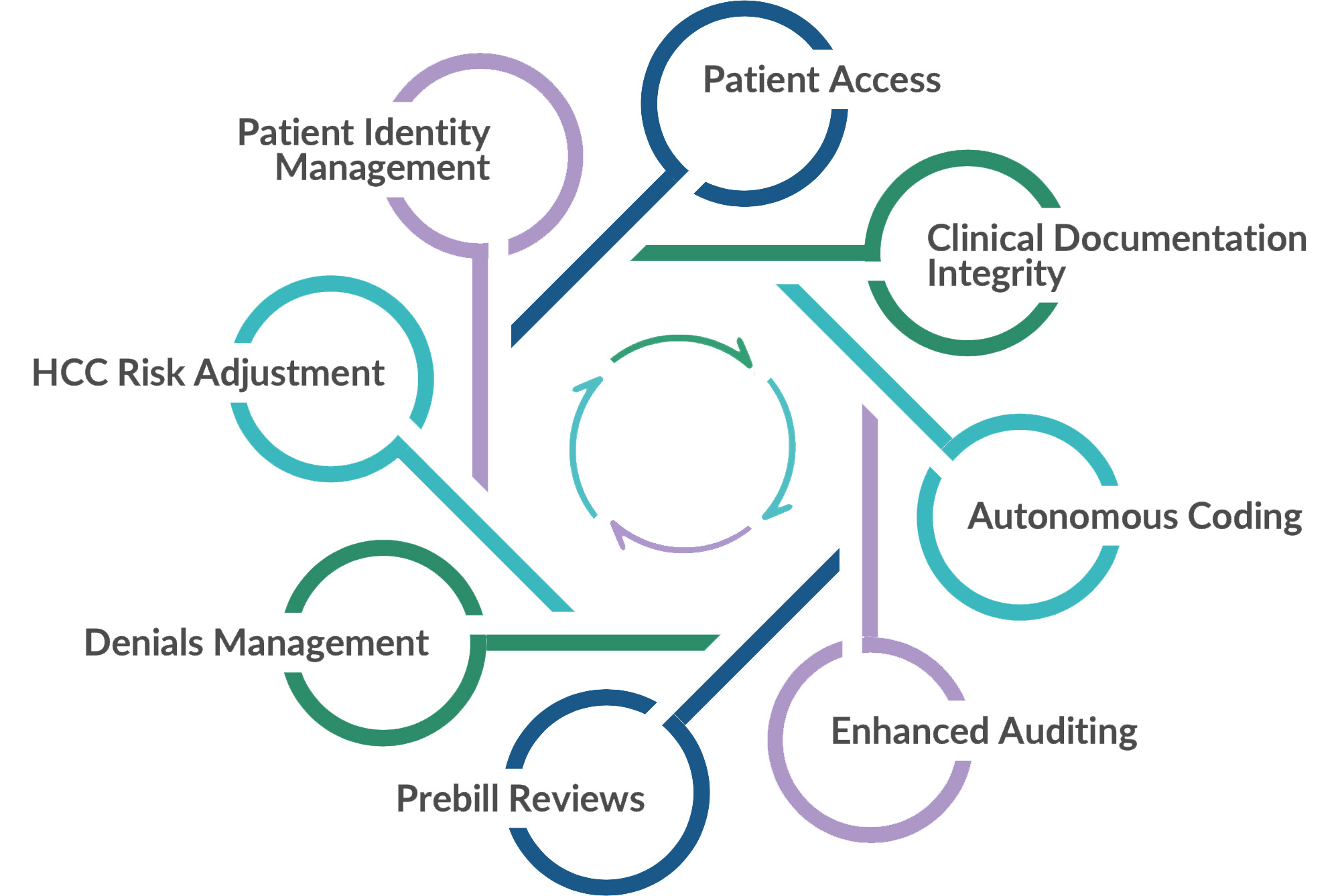
- Bots automate patient access processes.
- Ambient voice clinical documentation relieves clinical administrative burden.
- Autonomous coding processes high-volume, outpatient cases.
- ML reviews cases, conducts first-pass case audits, and dramatically expands audit sample size.
- AI prevents denials before billing by alerting teams to mismatches, errors, and more.
- AI automatically matches patient data and improves accuracy.
Trust but Verify: Four C-Suite Questions to Ask in Mid- Revenue Cycle
There are no experts yet for AI in healthcare, but there’s promise. The entire industry is learning together. However, several important considerations have recently emerged.
The following four questions help health executives vet technology and implementation partners for upcoming 2024 AI initiatives.
1. Speak with customers.
Ask what worked and what didn’t work. Closely review each customer’s implementation and integration processes with the vendor or implementation partner.
2. Verify mid-revenue cycle expertise.
Connect your internal teams with company experts to ensure potential partners possess a deep understanding of each unique business problem and have experience with your specific use case.
3. Shore up infrastructure.
Work with internal IT teams and potential AI partners to confirm the appropriate infrastructure exists to support the project.
4. Address data quality.
Assess current data for quality, accuracy, and bias to ensure outputs are valid and valuable. Best practice is to use large language models (LLMs) curated for medicine.
Case in Point: Automated Coding Requires Due Diligence
Coding is the most labor-intensive aspect of the mid-revenue cycle. Quality, capacity, throughput, and cycle time are all important considerations in medical record coding. Automated coding technology vendors strive to improve these key performance metrics.
Some succeed, but others don’t. The ones that do are using a strong mix of AI, process excellence, AND people to succeed.
Relying purely on technology with fully autonomous coding is a dangerous path. Furthermore, most automated coding solutions today can perform well for outpatient and ambulatory encounters while continuing to struggle with complex, inpatient cases.
“e4health is our trusted advisor to evaluate new and optimize existing solutions and walked us through a roadmap to ensure a practical approach for innovation. Their experts unlocked the power of technology in the mid-revenue cycle to achieve maximum results and desired outcomes.”
– VP Revenue Cycle, Large Academic Medical Center
Nuances for Automating the Mid-Revenue Cycle
The Team at e4health possess the health IT, health information, and revenue cycle expertise and experience to help your organization harness the power of AI safely, quickly, and effectively. By first assessing your revenue cycle readiness, our integrated teams serve as strategic automation advisors and executors across eight value areas.
Case in Point: Code Auditing and Informed CDI
Human coding auditors are limited by time in the volume of cases they are able to review. Consequently, potential denials slip through the cracks resulting in lost revenue or costly payer takebacks.
Bots can review every chart, identify gaps in clinical documentation or coding, escalate cases to human reviewers, and find patterns to improve documentation and coding over time.
“The goal of every e4health partnership with a customer is to build consistency, value, and quality across the revenue cycle continuum. AI, ML, and RPA enable mid-revenue cycle teams to manage by exception versus manual intervention. Team capacity increases with a combination of digital copilots and internal teams while leveraging both together to improve quality, productivity, and net realized revenue.”
– Matthew Zubiller, CEO, e4health
e4health Stands Ready to Lead
Getting started with AI, ML, or RPA is the most important decision HCOs can make right now. We suggest small, impactful steps toward solving important, specific business problems. Results should be demonstrated quickly in weeks versus months or years in alignment with the organization’s strategic priorities.
Finally, pay attention to the readiness of your organization. AI capabilities such as alerts, prompts, and nudges must be carefully integrated into legacy workflows. In addition, new skills and roles will emerge. This is especially true across legacy teams in mid-revenue cycle areas. Prepare your teams now for the changes ahead.
By partnering with e4health, HCOs ensure they receive maximum value and achieve their desired outcomes from new, and still evolving, technology investments.
Request a Mid-Revenue Cycle AI Assessment
The decisions you make around AI today will directly impact your organization’s future success. e4health helps you plan for and assess AI solutions to optimize your revenue cycle.
Measure Success in Mid-Revenue Cycle
- Define clear, practical, and realistic SMART goals for progress.
- Measure and track outcomes with KPIs such as return on investment, cost savings, cash acceleration, and revenue retention.
- Refine AI strategy based on results.
- Seek objective feedback and guidance from users.
- Assess, learn, and adapt as you progress to the next milestone, using the KPIs as your guide.
“Amidst the rapid evolution of technology, mastering change management is paramount. In the realm of emerging technologies, precision and diligence pave the path to success. ”
– David Van Doren, Partner & Board Member, e4health